Original version in Spanish: ¿Ha sido un fracaso la gestión española del COVID-19? Errores, lecciones y recomendaciones.
Summary
Spain has been one of the countries that has recorded the greatest impact of COVID-19 in the world, both in terms of infections and deaths, over the first half of 2020. The limited knowledge about the nature of the virus, the lack of a homogeneous and reliable counting method in the various countries, and the distinct rates at which the disease unfolded hinder comparisons and prevent the establishment of cast-iron certainties. Even with these reservations, and bearing in mind the information now available, it is possible to postulate certain hypotheses regarding the reasons that account for the severity of the disease’s spread in Spain.
The possible explanatory factors, which are manifold and complex, point to human geography (high population density and the intensity of foreign connections and domestic mobility, particularly as far as Madrid and Barcelona are concerned), demographics (ageing) and cultural habits (sociability and intergenerational cohabitation), but also to failings in the public health system. Notable among these are the lack of preparation and experience concerning pandemics in primary healthcare, hospital shortcomings, malpractice in many old peoples’ homes, less-than-ideal coordination between administrations and the delays in instituting social distancing measures.
The analysis also includes important positive aspects of the Spanish response (social resilience, comparatively strict application of the social distancing measures once they had been decreed, and the creditable performance of the health system outside the major cities), which ended up proving its effectiveness at flattening the infection curve in the second half of spring. The provisional conclusions seek to help in managing the easing of lockdown and to prepare for possible secondary outbreaks of coronavirus and other infections in the future.
How many cases, how many deaths
Five months have elapsed since the declaration of emergency issued by the World Health Organisation (WHO) and many aspects of COVID-19 remain as yet unknown. Its frequency and mortality are so varied and heterogeneous in terms of intensity and geography that, for now, there are no conclusive answers and this impedes any rigorous attempt to analyse the way different countries have managed it. However, although there remain unanswered questions about the nature and evolution of the pandemic and there are clear problems in the comparative counting of infections, as will be noted below, there are already enough elements to start to delve into the possible reasons for Spain having had so many cases and deaths.
According to the information reported by the countries themselves, Spain (which is the 30th largest country in the world in terms of population) was eighth in terms of absolute number of cases at the beginning of July 2020, behind the US, Brazil, Russia, India, Peru, Chile and the UK.2 However, bearing in mind the vertiginous rates at which coronavirus has spread recently in various non-European countries, it is highly likely that in coming months it will drop back several positions (and be overtaken by Mexico, Pakistan, South Africa, Iran, Saudi Arabia and possibly Bangladesh and Turkey). If measurement of the frequency of officially acknowledged cases is calculated relative to the population, Spain approaches the start of summer occupying the 15th position worldwide, behind various countries in the Persian Gulf and Latin America as well as the US, although consistently at the forefront in Europe (where only Luxembourg and Sweden exceed it).
The above statistics are, as mentioned, the officially acknowledged ones and it is imperative to view them with consummate care, both because of the scant transparency shown by some countries and because of the objective counting difficulties associated with an illness where a considerable proportion of infected patients show few symptoms or are asymptomatic. Moreover, there are enormous differences in the ability of national health systems to detect and quantify cases. Some (such as South Korea, Germany and Denmark) have shown greater efficiency when it comes to identifying infected patients in the initial phases of the epidemic, while others (such as the US, Russia, the UK and Spain itself) ramped up testing only when they became significantly affected, and finally there are those that have not been able to get even close to measuring the true extent of the pandemic. Whatever the case may be, and however cautiously the data are treated due to this widespread overburdening of capacities, there can be little doubt that Spain is at the forefront of COVID-19 incidence, at least in Europe, and this is also confirmed by the first studies into seroprevalence where, in theory, problems of undercounting are avoided.3
The questions and lack of homogeneity regarding the official information also arise when one turns to the number of deaths, a statistic that has understandably been viewed as more important for determining the real impact of the disease.4 Thus, according to the official statistics, at the beginning of July Spain ranked seventh in the world in terms of absolute number of deaths (below six more populous countries, namely the US, Brazil, the UK, Italy, France and Mexico). When the ranking is carried out relative to population size, and once micro-countries have been removed, Spain is ranked only behind Belgium and the UK. Here once again, as with the number of cases, the difficulties in gathering information cast doubt on the reliability of the international comparison of mortality rates. An alternative measurement to the official figures consists of taking, as a proxy indicator, the difference between the total deaths recorded and those expected based on historical trends for the same period. These contrasts reveal the scant credibility of the official information reported in some Asian and Latin American countries (in some cases, they barely account for 15% of the excess deaths actually occurring). In others, such as China, the problem is not the low capacity for managing records so much as opacity.
In Western countries the veracity of the data is greater. In some of them, such as Belgium and Germany, even suspect cases are counted, meaning that their official data and their excess deaths relative to the historical average almost converge. In others, where COVID-19 patients are deemed only to be people who have had a positive PCR or similar test result, such as Spain, Italy and the UK, the reported number of deaths due to the disease is around 60% of the total increase in deaths. Thus, as far as Spain is concerned, in the period from March to June 2020 rather more than 28,000 deaths were certified as owing to coronavirus, whereas the monitoring system of the Carlos III Health Institute (see Figure 1) recorded 43,000 excess deaths, which the National Statistics Institute raised to 48,000.
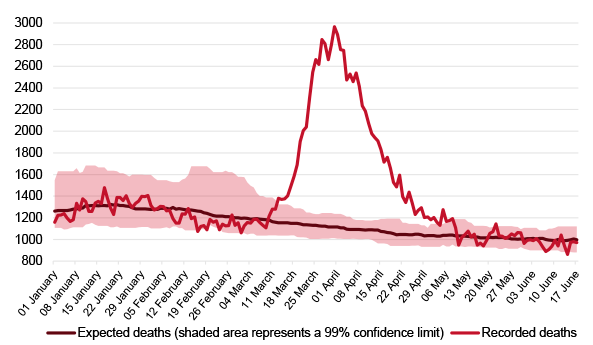
These attempts to control undercounting are still provisional and will vary as the records are updated and the course of the disease continues to unfold, particularly in non-Western countries. In the currently available figures there are already various Latin American countries (Peru, Ecuador) clearly placed above Spain, but if the comparison is restricted to countries in Europe, then Spain and the UK lead the actual excess deaths per capita, followed by Italy, Belgium, the Netherlands, Sweden, Switzerland and France respectively.5 Thus all the available data point to Spain being one of the countries in Europe, and at the start of summer also in the world, with the greatest incidence. What are the reasons for such a high position in the rankings of cases and deaths due to the virus?
Miguel Otero-Iglesias, Ignacio Molina & José Pablo Martínez
Elcano Royal Institute | @miotei, @_ignaciomolina & @jpmromera
1 Part of this text, now enlarged and updated, was published in the first sections of the jointly produced document by Charles Powell, Ignacio Molina & José Pablo Martínez (Coords.) (2020), España y la crisis del coronavirus: una reflexión estratégica en contexto europeo e internacional, Elcano Royal Institute, Madrid, June. The authors would like to thank in particular Carmen González Enríquez, whose contributions are evident in various passages of this analysis.
2 The source of official data used in this analysis is the European Centre for Disease Prevention and Control (ECDC), an EU agency.
3 See the comparative study carried out by scientists at Imperial College London, which calculates the real percentages of the infected population in selected European countries: Spain, with 5.5% of its population infected ranks only behind Belgium (8%) and ahead of the UK (5.1%), Italy (4.6%), Sweden (3.7%), France (3.4%) and Germany (0.9%). The official Spanish study into seroprevalence, carried out on the basis of a large sample, reported a final result of 5% immunity. See the article in The Lancet. These data suggest that some 2.5 million people in Spain have been infected, whereas the officially detected cases approach only 300,000.
4 The figure for deaths is more important than that of infections not only because of the human impact involved but also because it enables the management of the pandemic to be evaluated rather better. In the final analysis, a large number of infected patients, capable of being treated by the national health system, would gradually help to achieve so-called ‘herd immunity’. No country has adopted such a strategy but, despite this, many cases and few deaths would be an indicator of healthcare efficacy. There are no positive aspects, by contrast, of a high mortality rate.
5 Newspapers such as the New York Times, the Financial Times and El País have undertaken comparisons showing which countries reflect reality with vary degrees of precision. Prominent in Europe is the information provided by the EuroMOMO (European Mortality Monitoring) network, which is a system that sets out to track daily excess deaths in collaboration with the governments of 24 states, the ECDC and the WHO
Cleaning and disinfection of streets. Photo: Manuel (@manueljota)




